GENERAL DENTISTRY
1. DENTAL EXAM
- DENTAL CLEANING – PROPHYLAXIS
- DIGITAL X-RAY
- PERIODONTAL MAINTENANCE
- SCALING AND ROOT PLANING – DEEP CLEANING
- VELSACOPE ORAL PRECANCER AND CANCER
A professional dental cleaning (dental prophylaxis) is a cleaning procedure that thoroughly cleans the teeth. Cleanings are an excellent way to help keep the oral cavity in good health, and halt the progression of gum disease (gingivitis and periodontal disease).
Cleaning is recommended twice annually as a preventative measure, but should be performed every 3-4 months on sufferers from periodontal disease. Though periodontal disease cannot be completely reversed, cleaning is one of the tools the dentist can use that effectively halts its destructive progress.
Your cleaning appointment will include a comprehensive dental exam that offers several benefits:- Removal of plaque
Plaque is a sticky, almost invisible film that forms on the teeth. It is a growing colony of living bacteria, food debris and saliva. The bacteria produce toxins (poisons) that inflame the gums. This inflammation is the start of periodontal disease. - Removal of calculus (tartar)
Calculus is hardened plaque that has been left on the tooth for some time, and becomes firmly attached to the tooth surface. Calculus forms above and below the gum line. It can only be removed with special dental instruments, and can cause serious periodontal disease if left untreated. With even the best brushing and flossing homecare techniques, it can be impossible to remove debris, bacteria and deposits from gum pockets. The experienced eye of a dentist using specialized scaling tools and dental equipment is needed in order to spot and treat problems such as plaque and calculus buildup. - Teeth polishing
Remove stain and plaque that is not otherwise removed during tooth brushing and scaling. - Aesthetics
It is hard to feel confident about a smile marred by yellowing, stained teeth. Cleaning can rid the teeth of unsightly stains and return the smile to its former glory. - Fresher breath
Periodontal disease is often signified by persistent bad breath (halitosis). Bad breath is generally caused by a combination of rotting food particles below the gum line, possible gangrene stemming from gum infection, and periodontal problems. The removal of plaque, calculus and bacteria noticeably improves breath and alleviates irritation. - Identification of health issues
Many health problems first present themselves to the dentist. Since cleaning involves a thorough examination of the entire oral cavity, the dentist is able to screen for oral cancer, evaluate the risk of periodontal disease and often spot signs of medical problems like diabetes and kidney problems. Recommendations can also be provided for altering the home care regimen.
Cleaning can either be performed in the course of a regular dental visit or, if necessary, under general anesthetic. The latter is particularly common where severe periodontal disease is suspected or has been diagnosed by the dentist. An endotracheal tube is sometimes placed in the throat to protect the lungs from harmful bacteria that will be removed from the mouth.
Cleaning is generally performed in several stages:- Supragingival cleaning (scaling)
The dentist will thoroughly clean the area above the gum line with scaling tools to rid them of plaque and calculus. - Subgingival (deep) cleaning (scaling)
This is the most important step for patients with periodontal disease because the dentist is able to remove calculus from the gum pockets and beneath the gum line. - Root planing
This is the smoothing of the tooth root by the dentist to eliminate any remaining bacteria. These bacteria are extremely dangerous to periodontitis sufferers, so eliminating them is one of the top priorities of the dentist. - Medication
Following scaling and root planing, an antibiotic or antimicrobial cream is often placed in the gum pockets. These creams promote fast and healthy healing in the pockets and help ease discomfort.
Digital x-rays (digital radiography) is the latest technology used to take dental x-rays. This technique uses an electronic sensor (instead of x-ray film) that captures and stores the digital image on a computer. This image can be instantly viewed and enlarged helping the dentist and dental hygienist detect problems easier. Digital x-rays reduce radiation exposure by 80-90% compared to the already low exposure of traditional dental x-rays.
Dental x-rays are essential, preventative, diagnostic tools that provide valuable information not visible during a regular dental exam. Dentists and dental hygienists use this information to safely and accurately detect hidden dental abnormalities and complete an accurate treatment plan. Without x-rays, problem areas may go undetected.
Dental x-rays may reveal:- Abscesses or cysts.
- Bone loss.
- Cancerous and non-cancerous tumors.
- Decay between the teeth.
- Developmental abnormalities.
- Poor tooth and root positions.
- Problems inside a tooth or below the gum line.
Detecting and treating dental problems at an early stage may save you time, money, unnecessary discomfort, and your teeth!
Are dental x-rays safe?
We are all exposed to natural radiation in our environment. Digital x-rays produce a significantly lower level of radiation compared to traditional dental x-rays. Not only are digital x-rays better for the health and safety of the patient, they are faster and more comfortable to take, which reduces your time in the dental office. Also, since the digital image is captured electronically, there is no need to develop the x-rays, thus eliminating the disposal of harmful waste and chemicals into the environment.
Even though digital x-rays produce a low level of radiation and are considered very safe, dentists still take necessary precautions to limit the patient’s exposure to radiation. These precautions include only taking those x-rays that are necessary, and using lead apron shields to protect the body.
How often should dental x-rays be taken?
The need for dental x-rays depends on each patient’s individual dental health needs. Your dentist and dental hygienist will recommend necessary x-rays based upon the review of your medical and dental history, a dental exam, signs and symptoms, your age, and risk of disease.
A full mouth series of dental x-rays is recommended for new patients. A full series is usually good for three to five years. Bite-wing x-rays (x-rays of top and bottom teeth biting together) are taken at recall (check-up) visits and are recommended once or twice a year to detect new dental problems.
Periodontal disease can re-activate, as periodontal bacterial colonies begin to rebuild every 50–75 days. If you are diagnosed with periodontal disease, you need ongoing periodontal maintenance cleanings at least 4 times a year to prevent further bone loss and subsequent tooth loss.
Daily oral hygiene measures to prevent periodontal disease from worsening include:- Brushing.
Brushing properly on a regular basis (at least twice daily), with the patient attempting to direct the toothbrush bristles underneath the gum-line, to help disrupt the bacterial growth and formation of subgingival plaque. - Flossing.
Flossing daily and using interdental brushes (if there is a sufficiently large space between teeth), as well as cleaning behind the last tooth, the third molar, in each quarter. - Antiseptic Mouthwash.
Chlorhexidine gluconate based mouthwash in combination with careful oral hygiene may cure gingivitis, although they cannot reverse any attachment loss due to periodontal disease. - Soft Toothbrush.
Using a soft toothbrush to prevent damage to tooth enamel and sensitive gums.Medication. Using periodontal trays to maintain dentist-prescribed medications at the source of the disease. The use of trays allows the medication to stay in place long enough to penetrate the biofilms where the bacteria are found. - Check-Ups.
Regular dental check-ups and professional teeth cleaning at least 2-4 times per year. Dental check-ups serve to monitor the person’s oral hygiene methods and levels of attachment around teeth, identify any early signs of periodontal disease, and monitor response to treatment.
The objective of scaling & root planning is to remove etiologic agents which cause inflammation to the gingival (gum) tissue and surrounding bone. Common etiologic agents removed by this conventional periodontal therapy include dental plaque and tartar (calculus).
These non-surgical procedures which completely cleanse the periodontium, work very effectively for individuals suffering from gingivitis (mild gum inflammation) and moderate/severe periodontal disease.
Reasons for scaling and root planingScaling and root planning can be used both as a preventative measure and as a stand-alone treatment. These procedures are performed as a preventative measure for a periodontitis sufferer.
Here are some reasons why these dental procedures may be necessary:- Disease prevention.
The oral bacteria which cause periodontal infections can travel via the bloodstream to other parts of the body. Research has shown that lung infections and heart disease have been linked to periodontal bacteria. Scaling and root planing remove bacteria and halts periodontal disease from progressing, thus preventing the bacteria from traveling to other parts of the body. - Tooth protection.
When gum pockets exceed 3mm in depth, there is a greater risk of periodontal disease. As pockets deepen, they tend to house more colonies of dangerous bacteria. Eventually, a chronic inflammatory response by the body begins to destroy gingival and bone tissue which may lead to tooth loss. Periodontal disease is the number one cause of tooth loss in the developed world. - Aesthetic effects.
Scaling and root planing help remove tartar and plaque from the teeth and below the gumline. As an added bonus, if superficial stains are present on the teeth, they will be removed in the process of the scaling and root planning procedure. - Better breath.
One of the most common signs of periodontal disease is halitosis (bad breath). Food particles and bacteria can cause a persistent bad odor in the oral cavity which is alleviated with cleaning procedures such as scaling and root planing.
Scaling and root planing treatments are only performed after a thorough examination of the mouth. The dentist will take X-rays, conduct visual examinations and make a diagnosis before recommending or beginning these procedures.
Depending on the current condition of the gums, the amount of calculus (tartar) present, the depth of the pockets and the progression of the periodontitis, local anesthetic may be used.
- Scaling.
This procedure is usually performed with special dental instruments and may include an ultrasonic scaling tool. The scaling tool removes calculus and plaque from the surface of the crown and root surfaces. In many cases, the scaling tool includes an irrigation process that can also be used to deliver an antimicrobial agent below the gums that can help reduce oral bacteria. - Root planing.
This procedure is a specific treatment which serves to remove cementum and surface dentin that is embedded with unwanted microorganisms, toxins and tartar. The root of the tooth is literally smoothed in order to promote good healing. Having clean, smooth root surfaces helps bacteria from easily colonizing in future. Following these deep cleaning procedures, the gum pockets may be treated with antibiotics. This will soothe irritation and help the gum tissues to heal quickly.
During the next appointment, the dentist will thoroughly examine the gums again to see how well the pockets have healed. If the gum pockets still measure more than 3mm in depth, additional and more intensive treatments may be recommended.
Cancer is an abnormal disorganized growth of cells in the tissues of a person. Cancer cells keep on multiplying without paying heed to the body’s command to stop. This abnormal growth of cells destroys the normal structure and the function of the affected tissue and the body in general.
Any cancerous growth occurring within the the oral cavity is known as Oral Cancer. The oral cavity includes the mouth and all the structures within it, such as the tongue, teeth, gums, etc.
Among cancers, oral cancer is one of the most common causes of death.CAUSES
Cancer in the mouth does not occur overnight. It occurs as a series changes within the tissue, which eventually promote the development of cancer.
- Tobacco
- Alcohol
- Nutritional deficiencies
- Virus infection
- Sunlight
- Other miscellaneous factors such as trauma, heat, and irritation from sharp teeth, poorly restored fillings and ill-fitting dentures.
SIGNS & SYMPTOMS
Oral cancer may initially present without any symptoms. Patients are most often identified only after a significant progression of the disease. Discomfort is the most common symptom that compels a patient to seek medical care. A cancer patient may present with any of the following symptoms:
- Awareness of a mass present or growing within the oral cavity.
- Toothache.
- Pain in the ear.
- Limited mouth opening.
- Excessive bleeding which is not seen that commonly.
- A non-healing ulcer in the oral cavity.
- Swelling on the gums interfering with the seating of the dentures in the mouth.
A majority of oral cancers involve the tongue, the posterior region of the oral cavity and the floor of the mouth. The lips, gums, the under surface of the tongue and the palate (bones separating the mouth from the floor of the nose) are less frequently involved.
WARNING SIGNS
Certain pre-cancerous lesions occurring in the oral cavity may indicate the person’s susceptibility to cancer. These lesions can be in the form of
- White patches in the mucous membrane covering the oral cavity and along the lateral border of the tongue, which cannot be removed by rubbing the affected area.
- Red patches seen on the mucous membrane lining the mouth and the tongue.
- Increase in fibrous content of the mucous membrane lining the cheek, which presents itself as thick fibrous bands running along the inner aspect of the cheek.
DIAGNOSIS
1. Thorough examination of the oral cavity and the neck region conducted without neglecting any area may show hard lumps of tissues, which may indicate cancer. The patient is assessed for any suspicious tissue changes, which may include a white, red or a mixed white or red lesion.
2. Imaging the lesion using x-ray films, CT scan and advanced diagnostic techniques such as MRI helps in defining the location and extent of the cancerous growth.
3. Microscopic examination of a tissue specimen from the suspected lesion is the best method to confirm or rule out oral cancer. It gives the exact type and nature of cancer.
[ CT Scan: is an advanced diagnostic technique using x-rays to three-dimensionally identify the site and extent of a lesion.
MRI: It is more advanced technique, which uses magnetic force to diagnose both bony and soft tissue lesions.]
TREATMENT
The principle objective is to cure the patient of cancer. The choice of treatment depends upon factors such as cancer cell type, amount of changes in the cell-size and location of the cancerous growth.
Surgery or radiation is used with curative intent in treatment of cancer. Chemotherapy (Medicines) is used as an additional form of treatment. In an early lesion either surgery or radiation as a form of treatment would suffice. But in an advanced condition, a combination of both surgery and radiation is required.
There is rarely a second chance available for cure. Hence the initial approach of treatment is critical. The survival rates after early detection and treatment of cancer have been noted to be 70%. Chemotherapy (Medicines) is a weak substitute for the above-mentioned treatment.
More Information:
Tobacco utilization either in the form of smoking or chewing is an important factor in the development of oral cancer. About 97% of oral cancer victims are known to be associated with tobacco either in the form of smoking or chewing. Pipe smoking and cigar smoking have been known to increase the risk levels by a few folds. Among the various habits associated with tobacco, tobacco chewing is known to cause oral cancer more rapidly than any of the other habits. This is because of the direct and repeated contact of the tobacco with the mucous membrane of the oral cavity.
Do all betel nut or tobacco chewers get oral cancer?
Betel nut and tobacco chewers are definitely more prone to oral cancer than those who do not have this habit, but there are also other factors such as genetics, diet, environment and the person’s immune system.
Will stopping the habit improve the condition?
There are certain lesions seen frequently in the mouth of betel nut and tobacco chewers. These lesions precede oral cancer. If these preceding lesions are identified in time, then stopping the habit will definitely improve the lesion or maybe even cure it.
Is pain an early sign of cancer?
Not always. Pain is usually a late symptom of cancer. People often think that persistent pain such as headache or constant pain in the region of the face means cancer, but this is rarely the case. However pain should not be ignored.
What are the side effects of treatment?
There are side effects to all forms of treatments involving oral cancer.
-Surgery
If the lesion is small then there are usually no side effects, but if the lesion is large then it may require the removal of the affected structures resulting in the speech defects, difficulty in swallowing and also facial deformities. These conditions can rehabilitated by speech therapy and by physiotherapy.
- Radiation therapy
During and after radiation therapy the patient develops mouth sores. The patient also suffers from reduced secretion of saliva, which causes difficulty in swallowing and makes the patient more prone to tooth decay and other forms of infection.
-Chemotherapy
Side effects depend on the kind of drug used. The usual side effects are loss of hair, ulcers in the mouth and in the stomach, reduced resistance to infection, loss of appetite, nausea, vomitting, and lack of energy
2. RESTORATIVE
- DENTAL BONDING
- COMPOSITE WHITE FILLING
- DENTAL CROWNS (CAPS)
- DENTAL FIX BRIDGES
- DENTURES AND PARTIAL DENTURES
- INLAY AND ONLAY
- DENTAL IMPLANTS
Dental bonding is a procedure in which a tooth-colored resin material (a durable plastic material) is applied and hardened with a special light, which ultimately “bonds” the material to the tooth to restore or improve a person’s smile. Dental bonding is an option that can be considered for the following conditions:
- To repair decayed teeth (composite resins are used to fill cavities)
- To repair chipped or cracked teeth
- To the appearance of discolored teeth
- To close spaces between teeth
- To make teeth look longer
- To change the shape of teeth
- As a cosmetic alternative to amalgam fillings
- To protect a portion of the tooth’s root that has been exposed when gums recede
Little advance preparation is needed for dental bonding. Anesthesia is often not necessary unless the bonding is being used to fill a decayed tooth. Your dentist will use a shade guide to select a composite resin color that will closely match the color of your tooth.
Next, the surface of the tooth will be roughened and a conditioning liquid applied. These procedures help the bonding material adhere to the tooth. The tooth-colored, putty-like resin is then applied, molded, and smoothed to the desired shape. An ultraviolet light or laser is then used to harden the material. After the material is hardened, the dentist will further trim and shape it, and polish it to match the sheen of the rest of the tooth surface. Dental bonding takes about 30 to 60 minutes per tooth to complete.
What Are the Advantages and Disadvantages of Dental Bonding?Advantages:
Dental bonding is among the easiest and least expensive of cosmetic dental procedures. Unlike veneers and crowns, which are customized tooth coverings that must be manufactured in a laboratory, bonding usually can be done in one office visit unless several teeth are involved. Another advantage, compared with veneers and crowns, is that the least amount of tooth enamel is removed. Also, unless dental bonding is being performed to fill a cavity, anesthesia is usually not required.
Disadvantages:
Although the material used in dental bonding is somewhat stain resistant, it does not resist stains as well as crowns. Another disadvantage is that the bonding materials do not last as long nor are as strong as other restorative procedures, such as crowns, veneers, or fillings. Additionally, bonding materials can chip and break off the tooth. Because of some of the limitations of dental bonding, some dentists view it as best suited for small cosmetic changes, for temporary correction of cosmetic defects, and for correction of teeth in areas of very low bite pressure (for example, front teeth). Consult with your dentist about the best cosmetic approach for your particular problem.
Bonded teeth do not require special care. Simply follow good oral hygiene practices. Brush your teeth at least twice a day, floss at least once a day and see the dentist for regular professional check-ups and cleanings.
Because bonding material can chip, it is important to avoid such habits as biting fingernails; chewing on pens, ice, or other hard food objects; or using your bonded teeth as an opener. If you do notice any sharp edges on a bonded tooth or if your tooth feels odd when you bite down, call the dentist.
How Long Does Bonding Material Last?The lifespan of bonding materials for your teeth depends on how much bonding was done and your oral habits. Typically, however, bonding material lasts from 3 years up to about 10 years before needing to be touched up or replaced.
Restoring a tooth includes replacing mercury silver amalgam fillings with composite white fillings in our holistic mercury free mercury safe practice. A composite (tooth colored) filling is used to repair a tooth that is affected by decay, cracks, fractures, etc. The decayed or affected portion of the tooth will be removed and then filled with a composite filling.
There are many types of filling materials available, each with their own advantages and disadvantages. You and the Doctor can discuss the best options for restoring your teeth.
Composite fillings, along with mercury silver amalgam fillings, are the most widely used today. However, because they are considered toxic with serious side effects, we do not use mercury silver amalgam fillings in our holistic practice. Not only will the safest and highest quality white Nano-hybrid resin that we use enhance your smile, but they will eliminate the potentially harmful old fashioned toxic heavy metal mercury silver amalgam fillings. In laboratory tests, these new state-of-the-art fillings strengthened teeth 7 to 8 times. Looking better never felt so good!
Because composite fillings are tooth colored, they can be closely matched to the color of existing teeth, and are more aesthetically suited for use in front teeth or the more visible areas of the teeth. As with most dental restorations, composite fillings are not permanent and may someday have to be replaced. They are very durable, and will last many years, giving you a long lasting, beautiful smile.
- Chipped teeth.
- Closing space between two teeth.
- Cracked or broken teeth.
- Decayed teeth.
- Worn teeth.
Composite fillings are usually placed in one appointment. While the tooth is numb, your dentist will remove decay as necessary. The space will then be thoroughly cleaned and carefully prepared before the new filling is placed. If the decay was near the nerve of the tooth, a special medication will be applied for added protection. The composite filling will then be precisely placed, shaped, and polished, restoring your tooth to its original shape and function.
It is normal to experience sensitivity to hot and cold when composite fillings are first placed, however this will subside shortly after your tooth acclimates to the new filling. You will be given care instructions at the conclusion of your treatment. Good oral hygiene practices, eating habits, and regular dental visits will aid in the life of your new fillings.
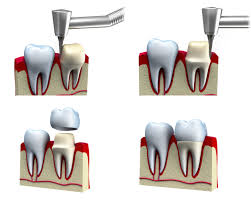
A crown is a type of dental restoration that, when cemented into place, fully cups over that portion of a tooth that lies at and above the gum line. Since it encases the entire visible aspect of a tooth, a dental crown, in effect, becomes the tooth's new outer surface. In comparison, dental fillings are restorations that fill in or patch just a portion of a tooth. Other terms that are used to refer to crowns are "dental caps" and "tooth caps". Crowns can be made out of porcelain, metal (a gold or other metal alloy), or a combination of both (porcelain-fused-to-metal).
Reasons for crowns:- Broken or fractured teeth.
- Cosmetic enhancement.
- Decayed teeth.
- Fractured fillings.
- Large fillings.
- Tooth has a root canal.
A crown procedure usually requires two appointments. Your first appointment will include taking several highly accurate molds (or impressions) that will be used to create your custom crown. A mold will also be used to create a temporary crown which will stay on your tooth for approximately two weeks until your new crown is fabricated by a dental laboratory. While the tooth is numb, the dentist will prepare the tooth by removing any decay and shaping the surface to properly fit the crown. Once these details are accomplished, your temporary crown will be placed with temporary cement and your bite will be checked to ensure you are biting properly.
At your second appointment your temporary crown will be removed, the tooth will be cleaned, and your new crown will be carefully placed to ensure the spacing and bite are accurate. You will be given care instructions and encouraged to have regular dental visits to check your new crown.
A dental bridge is a fixed (non-removable) appliance and is an excellent way to replace missing teeth.
There are several types of bridges. You and your dentist will discuss the best options for your particular case. The “traditional bridge” is the most popular type and is usually made of porcelain fused to metal. Porcelain fixed bridges are most popular because they resemble your natural teeth. This type of bridge consists of two crowns that go over two anchoring teeth (abutment teeth) and are attached to pontics (artificial teeth), filling the gap created by one or more missing teeth. Dental bridges are highly durable and will last many years, however they may need replacement or need to be re-cemented due to normal wear.
Reasons for a fixed bridge:- Fill space of missing teeth.
- Maintain facial shape.
- Prevent remaining teeth from drifting out of position.
- Restore chewing and speaking ability.
- Restore your smile.
- Upgrade from a removable partial denture to a permanent dental appliance.
Getting a bridge usually requires two or more visits. While the teeth are numb, the two anchoring teeth are prepared by removing a portion of enamel to allow for a crown. Next, a highly accurate impression (mold) is made which will be sent to a dental laboratory where the bridge will be fabricated. In addition, a temporary bridge will be made and worn for several weeks until your next appointment.
At the second visit, your permanent bridge will be carefully checked, adjusted, and cemented to achieve a proper fit. Occasionally your dentist may only temporarily cement the bridge, allowing your teeth and tissue time to get used to the new bridge. The new bridge will be permanently cemented at a later time.
You will receive care instructions at the conclusion of the procedure. Proper brushing, flossing and regular dental visits will aid in the life of your new permanent bridge.

A denture is a removable dental appliance replacement for missing teeth and surrounding tissue. They are made to closely resemble your natural teeth and may even enhance your smile. There are two types of dentures - complete and partial dentures. Complete dentures are used when all of the teeth are missing, while partial dentures are used when some natural teeth remain. A Partial denture not only fills in the spaces created by missing teeth, it prevents other teeth from shifting. A Complete denture may be either “conventional” or “immediate”. A conventional type is made after the teeth have been removed and the gum tissue has healed, usually taking 4 to 6 weeks. During this time the patient will go without teeth. Immediate dentures are made in advance and immediately placed after the teeth are removed, thus preventing the patient from having to be without teeth during the healing process. Once the tissues shrink and heal, adjustments will have to be made.
Dentures are very durable appliances and will last many years, but may have to be remade, repaired, or readjusted due to normal wear. Reasons for dentures:
- Complete Denture – Loss of all teeth in an arch.
- Partial Denture – Loss of several teeth in an arch.
- Enhancing smile and facial tissues.
- Improving chewing, speech, and digestion.
The process of getting dentures requires several appointments, usually over several weeks. Highly accurate impressions (molds) and measurements are taken and used to create your custom denture. Several “try-in” appointments may be necessary to ensure proper shape, color, and fit. At the final appointment, your dentist will precisely adjust and place the completed denture, ensuring a natural and comfortable fit.
It is normal to experience increased saliva flow, some soreness, and possible speech and chewing difficulty, however this will subside as your muscles and tissues get used to the new dentures.
You will be given care instructions for your new dentures. Proper cleaning of your new dental appliance, good oral hygiene, and regular dental visits will aid in the life of your new dentures.
Dental inlays and onlays are restorations used to repair rear teeth with mild to moderate decay or cracked and fractured teeth that are not sufficiently damaged to need a crown.
Ideal candidates for inlay or onlay work typically have too much damage or decay in the tooth structure to be successfully treated using a filling, but have sufficient healthy tooth remaining to avoid the need for a crown. This allows the dentist to conserve more of the patient’s original tooth structure.
They help to strengthen teeth by up to 75 percent, unlike traditional metal fillings which can actually reduce the strength of the teeth by up to 50 percent.
Inlays and onlays prolong tooth life and prevent the need for more dental treatment in the future.
Dental inlays and onlays are used when old fillings need to be removed or replaced. A dental inlay is similar to a filling and fits inside the cusp tips (top edges) of the tooth. A dental onlay is more extensive and extends over the cusps of the treated tooth.
During treatment the dentist removes the old fillings under local anesthesia and takes an impression of the tooth, which is sent to the dental laboratory. The new inlay or onlay is made from this mold in porcelain, metal, gold or composite resin material. The inlay or onlay is then cemented into place at the next appointment. The inlay or onlay blends successfully with the treated tooth and the rest of the teeth to achieve a natural, uniform appearance.
How are inlays and onlays done?It takes two appointments for the inlays and onlays treatment to be completed and to be finally bonded to the damaged area of the tooth.
Inlays and onlays are performed using very similar procedures. At the first appointment, your dentist begins the procedure by numbing the area to be treated with local anesthetic. Any decay or damage is removed by drilling, which cleans and prepares the tooth for the dental inlay or onlay. Using a small tray filled with dental putty that fits over the teeth, the dentist takes a mold (impression) of the damaged tooth. This impression is sent off to the dental laboratory, where a dental inlay or onlay is created that will fit your tooth exactly. Inlays and onlays are usually made from porcelain, which often most closely matches the normal color of the tooth, but they can also be made from composite resin or gold. While the inlay or onlay is being created at the lab, the dentist creates a temporary restoration (cover or filling) for your tooth to protect it until your next appointment.
At the second appointment, your dentist will remove the temporary restoration and then take time to ensure the inlay or onlay fits correctly. Only when the inlay or onlay fits perfectly will the dentist bond the inlay or onlay to the tooth with a strong resin adhesive. The inlay and onlay treatment is completed with a polish to ensure a smooth and aesthetically pleasing finish.
Each visit to the dentist for inlay or onlay treatment takes about an hour, with the first appointment taking slightly longer due to the preparation process. There will probably be a little discomfort after the inlay or onlay procedure, and the new tooth surface may feel a little odd, but you soon get used to the new tooth surface and how it feels and looks in your mouth. The tissue around the treated tooth may feel sore or sensitive, but this should subside in a couple of days. If you do feel some discomfort, you can take over-the-counter pain medication to alleviate the symptoms.


Despite improvements in dental care, dental implants are replacement tooth roots. Implants provide a strong foundation for fixed (permanent) or removable replacement teeth that are made to match your natural teeth.
Dental implants offer a natural solution to replace teeth lost due to trauma, decay, disease or old age. Replacing missing teeth improves the oral health as well as the functionality of the teeth, enhances smile and self-esteem. A dental implant is a small titanium screw root, which is fitted into the socket of the missing teeth that looks and functions like the real ones and can be used to replace a single tooth or several teeth.
The missing teeth can be replaced immediately by placing the implants directly into the available bone. With the use of angled, and/or max implant technology, is less likely to require bone grafting.
What Are the Advantages of Dental Implants?There are many advantages to dental implants, including:
- Improved appearance:
Dental implants look and feel like your own teeth. And because they are designed to fuse with bone, they become permanent. - Improved speech:
With poor-fitting dentures, the teeth can slip within the mouth causing you to mumble or slur your words. Dental implants allow you to speak without the worry that teeth might slip. - Improved comfort:
Because they become part of you, implants eliminate the discomfort of removable dentures. - Easier eating:
Sliding dentures can make chewing difficult. Dental implants function like your own teeth, allowing you to eat your favorite foods with confidence and without pain. - Improved self-esteem:
Dental implants can give you back your smile and help you feel better about yourself. - Improved oral health:
Dental implants don’t require reducing other teeth, as a tooth-supported bridge does. Because nearby teeth are not altered to support the implant, more of your own teeth are left intact, improving long-term oral health. Individual implants also allow easier access between teeth, improving oral hygiene. - Durability:
Implants are very durable and will last many years. With good care, many implants last a lifetime. - Convenience:
Removable dentures are just that; removable. Dental implants eliminate the embarrassing inconvenience of removing dentures, as well as the need for messy adhesives to keep them in place.
Success rates of dental implants vary, depending on where in the jaw the implants are placed but, in general, dental implants have a success rate of up to 98%. With proper care (see below), implants can last a lifetime. Can Anyone Get Dental Implants?
In most cases, anyone healthy enough to undergo a routine dental extraction or oral surgery can be considered for a dental implant. Patients should have healthy gums and enough bone to hold the implant. They also must be committed to good oral hygiene and regular dental visits. Heavy smokers, people suffering from uncontrolled chronic disorders-such as diabetes or heart disease- or patients who have had radiation therapy to the head/neck area need to be evaluated on an individual basis. If you are considering implants, talk to your dentist to see if they are right for you.
Our Implants are the clear choice for patients seeking fast, efficient and high quality dental implant services, performed only by highly trained and experienced dentist.